What are they?
What benefits can they bring?
What is their scope of practice?
Is funding available for them?
Are there any case studies?
What characteristics, training / qualifications, and competencies should they have?
Are there any requirements to receive ARRS funding?
What employment routes are there?
Any example job descriptions?
What clinical supervision do they need?
What should practice induction include?
What ongoing support is available for SPLWs?
What are social prescribing link workers (SPLWs)?
Social prescribing link workers (SPLWs) serve in a non-clinical capacity to help patients and service users take control of their health and wellbeing; they support individuals in creating a shared plan based on ‘what matters’ to them, and to help them connect with local community and voluntary groups and build up their confidence.
Additionally, SPLWs assist local community groups and services in becoming more accessible and sustainable, and support the formation of new ones. They are employed for their listening skills, empathy, and ability to support others.
SPLWs work with a wide range of people, including:
- Those who are lonely or isolated
- Those who need support with their mental health
- Those with complex social needs
- Those with one or more long-term conditions
For more information:
Induction Guide for Social Prescribing Link Workers
Provided by NHS England & NHS Improvement (NHSE / I), this document serves an induction guide for social prescribing link workers (SPLWs) starting employment in a primary care network.
To read it, please click here.
Why a Social Prescribing Link Worker?
One in five GP appointments focus on wider social needs[1], rather than acute medical issues. In areas of high deprivation, many GPs report that they spend significant amounts of time dealing with the consequences of poor housing, debt, stress and loneliness. Social prescribing and community-based support is part of the NHS Long Term Plan’s commitment to make personalised care business as usual across the health and care system and to bring additional capacity into the multi-disciplinary team. This approach aims to reduce pressure on clinicians, improve people’s lives through improved and timely access to health services and strengthen community resilience, meeting the needs of our diverse and multi-cultural communities.
Social prescribing enables all primary care staff and local agencies to refer people to a link worker and supports self-referral. Working under supervision of a GP, link workers give people time and focus on what matters to the person, as identified through shared decision making or personalised care and support planning. They will manage and prioritise their own caseload in accordance with the health and wellbeing needs of their local population, and where required discuss and/or refer people back to other health professionals and GPs in the PCN. They also connect people to local community groups and agencies for practical and emotional support. Link workers work within multi-disciplinary teams and collaborate with local partners to support community groups to be accessible and sustainable and help people to start new groups and activities.
Social prescribing can support a wide range of people, including (but not exclusively) people:
- with one or more long term conditions
- who need support with their mental health
- who are lonely or isolated
- who have complex social needs which affect their wellbeing.
There is emerging evidence that social prescribing can lead to a range of positive health and wellbeing outcomes for people, such as improved quality of life and emotional wellbeing.[2] Whilst there is a need for more robust and systematic evidence on the effectiveness of social prescribing,[3] social prescribing schemes may lead to a reduction in the use of NHS services,[4] including GP attendance. 59% of GPs think social prescribing can help reduce their workload.[5]
[1] Citizens Advice policy briefing (2015), A very general practice: How much time do GPs spend on issues other than health?
[2] Dayson, C. and Bashir, N. (2014), The social and economic impact of the Rotherham Social Prescribing Pilot. Sheffield: Sheffield Hallam University: https://www4.shu.ac.uk/research/cresr/sites/shu.ac.uk/files/socialeconomic–impact–rotherham.pdf
[3] Bickerdike, L., Booth, A., Wilson, P.M., et. Al. (2017), Social prescribing: less rhetoric and more reality. A systematic review of the evidence, BMJ Open 2017;7: e013384. doi: 10.1136/bmjopen-2016-013384
[4] Polley, M. et al. (2017), A review of the evidence assessing impact of social prescribing on healthcare demand and cost implications. London: University of Westminster
[5] RCGP (2018), Spotlight on the 10 High Impact Actions: http://www.rcgp.org.uk/about–us/news/2018/may/rcgpcalls–on–government–to–facilitate–social–prescribing–for–all–practices.aspx (accessed 2 June 2018)
SPLW Ref Guide
What benefits can SPLWs bring?
Principally, social prescribing link workers (SPLWs) can help to ease the workload and release time for GPs and general practice nurses (GPNs), by consulting with patients that do not have an immediate need for medical or nursing attention. In fact, 1-in-5 patients come to practice appointments with a non-clinical issue, which SPLWs can also be better-equipped to deal with.
There is evidence that social prescribing can lead to a number of positive health and wellbeing outcomes, including a better quality of life and emotional wellbeing. When implemented properly, SPLWs can support patients and service users in easily connecting with an assortment of local groups and services, including (but not limited to):
- Hospital discharge teams
- Fire services
- Police services
- Job centres
- Social care services
- Housing associations
- Voluntary, community, and social enterprise (VCSE) organisations
What is their scope of practice?
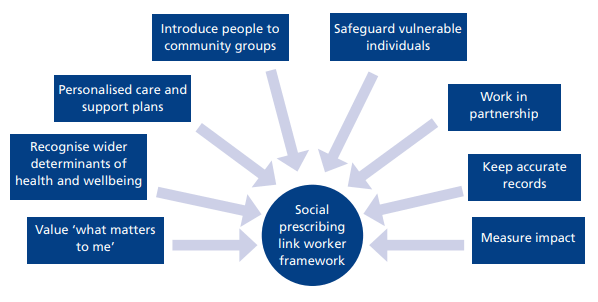
Below is a list of but some of a social prescribing link worker’s (SPLW) key tasks, quoted from NHSE / I’s Social Prescribing Summary Guide.
For a fuller account of their scope of practice, please be sure to consult the guide itself, linked below.
- Promoting social prescribing, its role in self-management, and the wider
determinants of health - Build relationships with key staff in GP practices within the local Primary Care Network (PCN), attending relevant meetings, becoming part of the wider network team, giving information and feedback on social prescribing
- Be proactive in developing strong links with all local agencies to encourage referrals, recognising what they need to be confident in the service to make appropriate referrals
- Work in partnership with all local agencies to raise awareness of social
prescribing and how partnership working can reduce pressure on statutory
services, improve health outcomes and enable a holistic approach to care - Provide referral agencies with regular updates about social prescribing, including training for their staff and how to access information to encourage appropriate referrals
- Seek regular feedback about the quality of service and impact of social
prescribing on referral agencies - Be proactive in encouraging self-referrals and connecting with all local
communities, particularly those communities that statutory agencies may find hard to reach - Meet people on a one-to-one basis, making home visits where appropriate within organisations’ policies and procedures. Give people time to tell their stories and focus on ‘what matters to me’. Build trust with the person, providing non-judgemental support, respecting diversity and lifestyle choices. Work from a strength-based approach focusing on a person’s assets
- Be a friendly source of information about wellbeing and prevention approaches
- Help people identify the wider issues that impact on their health and wellbeing, such as debt, poor housing, being unemployed, loneliness and caring responsibilities
NHSE / I Social Prescribing and Community-Based Support Summary Guide
Provided by NHS England & NHS Improvement (NHSE / I), this document is intended to outline what good social prescribing looks like and assist in implementing it.
To read it, please click here.
Is funding available for them?
Social prescribing link workers (SPLWs) are one of the Additional Roles Reimbursement Scheme (ARRS) roles, and therefore PCNs can receive funding for employing them.
According to NHS England & NHS Improvement (NHSE / I), PCNs will be able to receive reimbursement for 100% of the role’s actual full-time equivalent salary, plus employer on-costs (NI and pension) and a contribution.
For more information:
Network Contract Directed Enhanced Service: Additional Roles Reimbursement Scheme Guidance
Provided by NHS England & NHS Improvement (NHSE / I), this guidance document provides information on the Additional Roles Reimbursement Scheme (ARRS).
To read it, please click here.
This is custom heading element
Provided by NHS England & NHS Improvement (NHSE / I), this document is intended to outline what good social prescribing looks like and assist in implementing it.
To read it, please click here.
Are there any case studies?
As it turns out, NHSE / I have helpfully put together a page full of case studies for the social prescribing link worker (SPLW) role.
To access it, please use the button below.
What employment routes are there?
As it turns out, NHSE / I have helpfully put together a page full of case studies for the social prescribing link worker (SPLW) role.
To access it, please use the button below.
What can a Social Prescribing Link Worker do?
Social Prescribing Link Workers give people time and focus on what matters to the person as identified in their care and support plan. They connect people to community groups and agencies for practical and emotional support and offer a holistic approach to health and wellbeing, hence the name ‘social prescribing’.
Social prescribing enables patients referred by general practice, pharmacies, multi-disciplinary teams, hospital discharge teams, allied health professionals, fire service, police, job centres, social care services, housing associations and voluntary, community and social enterprise (VCSE) organisations get the right care for them.
Link workers typically work with people over 6-12 contacts (including phone calls and face to face meetings) over a three-month period with a typical caseload of up to 250 people, depending on the complexity of people’s needs.
NHS England Link
The above information can be found at NHS England » Expanding our workforce
Previous relevant experience
Although these are not strict as a guide, relevant experience might include the following:
- Worked with people with support needs previously in a key worker/ case manager type role and those who have a broad understanding of the wider determinants of health
- Supported and motivated people to make changes in their lives, helping the person to make plans based on what matters to them
What patients would be suitable to be referred to a SPLW?
Social prescribing works for a wide range of people, including people:
- with one or more long-term conditions
- who need support with their mental health
- who are lonely or isolated
- who have complex social needs which affect their wellbeing.
From a GP perspective practice teams should consider those patients that are frequent attenders with often unexplained physical symptoms, social isolation, mental health difficulties, and poorly controlled long-term conditions.
What’s the difference between social prescribing and active signposting?
“Active signposting” schemes generally involve existing staff in general practices, libraries and other agencies providing information to signpost people to community groups and services, using directories and local knowledge. They offer a light touch approach which works best for people who are confident and skilled enough to find their own way to community groups.
Social prescribing is different in that it focuses its support on people who lack the confidence or knowledge to approach other agencies or to get involved in community groups on their own. The personalised support of social prescribing link workers gives people time and confidence to work on the underlying issues which affect their health and wellbeing.
SPLW Ref Guide
Any Sample Case Studies?
A primary care navigator helped John to get his life back and address his ongoing health and social needs
Case study summary
John’s Primary Care Navigator talks about how he accessed a social prescribing primary care navigator via his GP after the death of his mum and losing his job. After working out what matters to John she was able to help him address his critical health, mental and financial issues, including now accessing benefits and services he was entitled to and other medical support.
John is in his mid 60’s. He lives alone in a two bedroom flat situated in a tower block, which was left to him by his mother who sadly died in 2013. Since then, John’s health had deteriorated. As well as poor control of his chronic diseases he then began to suffer from depression after the loss of his mother and being made redundant.
John was referred to the primary care navigator via his GP to see if we could help him in anyway. At first John was reluctant to engage with the primary care navigator as he felt embarrassed and lost and at an all-time low. We asked John if he would like to pop in for an informal chat, we made this on a regular basis. We began to build a relationship of trust and John began to communicate to us with ease.
He had cared for this mother and his benefits were all stopped when she died, to the point that he could not buy food. John suffered mentally and financially.
Over a period of eight months, we worked alongside foodbanks, The Salvation Army, The Green Doctor, Age UK and Citizens Advice Bureau and worked hard to make sure he could access the benefits and services he was entitled to. This enabled us to support John with food, clothes, paying off debts and energy efficient items for the home.
We also supported John in benefit advice and eventually won his appeal to unblock his benefit of £50 so he could feed himself. We then provided providing crucial medical information which helped to unlock another benefit and the funding was then backdated. It also now entitled him to other benefits too.
All this meant that he could now continue to live in his own house and look after himself. His health has improved and is now in control. John now looks forward to his weekly meet at the local Luncheon Club.
John keeps thanking us for all we did for him but if we did not have access to social prescribing then it would not have been possible to achieve what has been done. John knows that we will always be available if he needs us.
NHSE Case Study
The above case study was found here: NHS England » A primary care navigator helped John to get his life back and address his ongoing health and social needs
A day in the life of a SPLW?
The following ‘day in the life’ was sourced from a case study from another social prescribing organisation (see web link below):
AS PART OF ELEMENTAL’S MISSION TO SHINE A LIGHT ON SOCIAL PRESCRIBING AND HIGHLIGHT ALL THE GREAT WORK TO THAT TAKES PLACE ACROSS THE FORWARD THINKING AND INSPIRING ORGANISATIONS THAT WE WORK WITH, OUR NEW ‘DAY IN THE LIFE OF’ FEATURE AIMS TO RAISE AWARENESS OF THE PEOPLE ON THE GROUND THAT ARE EMPOWERING COMMUNITIES AND CHANGING LIVES THROUGH SOCIAL PRESCRIBING.
In our first feature, Rachel Studzinski, SPRING Social Prescribing Development worker for Health in Mind, a mental health and wellbeing charity in Scotland, explains more about her role as a link worker
ABOUT SPRING
The SPRING social prescribing programme is a community led and holistic approach to wellbeing in the Scottish Borders. My role is to support people to identify what is important to them and how they can make positive changes in their lives to achieve their goals through accessing local services, groups and activities.
No two days are ever the same, and I split my time between working from the different Health in Mind offices in our communities and getting out and about to talk to as many people as possible about social prescribing and how our programme can support a wide range of people working in health and wellbeing.
For example, I have been working with midwives in the area to raise awareness of our programme and its potential to support new mums with some of the challenges they face.

CREATING A SOCIAL PRESCRIBING CULTURE
This awareness raising work is really important because I spend a lot of my time trying to track down the right people in the NHS. There is a real communication job to do with social prescribing for anyone trying to reach in and we know that to tackle this need to go out into the community and not wait for people to come to us.
It’s so vital that we have NHS professionals on board to deliver social prescribing to its full potential, and to do that we need to create a new mindset that really understands how the social model can complement and enhance medical models.
The NHS might be the gateway, but it’s all about bridging the gap between statutory and non-statutory services, this is where the success to social prescribing lies and we need to work hard to create this culture.
We are lucky in the Borders that there’s a lot of support for social prescribing in the NHS, but we know that this is not a nationwide experience and I think the sector needs to work to avoid the ‘postcode lottery’ effect where it’s an option available to some but not others.

WORKING WITH GP PRACTICES
A large part of my work involves working with GP practices as this is the primary route of our referrals to the programme.
We have 13 GP practices signed up at the moment, with two more coming on board in the next few months. Some practices refer more than others, but all referrals come to us through Elemental’s social prescribing platform, which makes it so quick and easy for us.
We receive referrals through the Elemental system directly from the GP in real time, enabling me to respond quickly and set up appointments within a week.
TAKING TIME TO ASSESS PEOPLE’S NEEDS
The first step in any social prescribing referral is to go and meet the patient and have an hour to an hour and a half assessment where we look at each area of their life to identify where they want support and what they want to change in their lives. While this part of the assessment is fairly clinical at this stage, it’s important because this is what translates back for statutory services.
Once that is completed, I always add a personal goal in, which can be anything from ‘I would like to feel less isolated’, to ‘I would like to feel more confident’. Then we work together to do a smart goal around that which enables us to find the right social prescribing activity for them.
Once we have an idea of what they are looking for we can start to suggest things that are happening in their areas for them to try. As a link worker I see my role as facilitating what the social prescription might be, but really empowering the individual to choose the activities that work for them, whether that’s learning something new, ice skating, swimming or even sky diving!

SEEING THE DIFFERENCE
The most rewarding part of my role is seeing people thrive as they go through the programme.
For example, a lady I have been working with was referred to the programme for weight management after she’d been to different wellbeing teams who thought that they’d done all they could and after assessing her diet, felt that she needed to be referred into exercise classes.
However, through our referral we realised her needs were completely different. Through my initial assessment we identified that she had been diagnosed with arthritis and had a history of depression. She had been prescribed steroids which were causing her to gain weight, which was impacting on her confidence and triggering her depression. This in turn was affecting her relationship with her husband and her son. It was a real cyclical effect that was causing her to feel isolated.
She realised that she needed to change this cycle so together we developed her plan and I was able to look at activities to support her. She felt that she couldn’t go to the gym because of the pain it caused her knees, so I suggested swimming.
Getting a swimming costume was a big deal for her because of her body image challenges and it took us two or three weeks to overcome that, through lots of reassurance and text message conversations, and I was delighted when she text me one day to say she’d got a costume in the brightest colour she could find!
From there, we went swimming together. By the end of the 12 interventions that SPRING offered, she’d reached 76 lengths and was reporting that she’d lost five pounds, had started gardening at home again which she’d previously had to stop because of the pain caused by her arthritis, and found that her relationships were improving.
She was also able to walk longer distances before experiencing pain, particularly when shopping.
For me, this is a shining example of social prescribing in action.
THE FUTURE OF SOCIAL PRESCRIBING
The future is bright for social prescribing and link workers have a pivotal role to play in enabling it to fulfil its potential.
Developing partnerships will continue to be crucial, particularly in the voluntary sector where resources are tight. This is something that we need to continue to focus on, as well as developing that culture change within the NHS, whilst not losing sight of the fact that social prescribing must always be community led to be successful, whatever the pathway.
Volunteering is also an area at SPRING that I am working to develop. I’ve realised that I can’t fit every personality type of people that might be referred to us, and we need to continue to offer people diversity, and so I am currently recruiting volunteers to support this, which is proving a big success.
The more we can raise awareness of the real difference that community led social prescribing initiatives can make, the more lives we’ll be able to change and I’m really excited for what lies ahead for our work.

Rachel Studzinski, Health in Mind, SPRING Social Prescribing Development Worker
Rachel is passionate about equality and supporting social change that drives equality. She is the Health in Mind, Spring Social Prescribing Development Worker in the Scottish Borders. Heer role involves working collaboratively with primary care to offer non-medical interventions to patients.
A day in the life of a SPLW weblink
What characteristics, training / qualifications, and competencies should they have?
There are no formal qualifications or competencies required to become a social prescribing link worker (SPLW). However, it is recommended that one has the following:
- An understanding of the wider determinants of health, including social, economic, and environmental factors, and their effect on individuals, communities, and families
- Demonstrable commitment to professional and personal development
- Experience of partnership / collaborative working, and of building relationships across a variety of organisations
- Experience of working directly in a community development context, adult health and social care, learning support or public health / health improvement (including unpaid work)
- Knowledge of the personalised care approach
- NVQ Level 3, Advanced level or equivalent qualifications or working towards (recommended by NHS, but entirely up to local partners whether or not this is included, so you may want to check)
- Training in motivational coaching and interviewing, or equivalent experience
Additionally, NHS Careers recommend that SPLWs possess the following characteristics:
- Excellent listening and communication skills
- Empathy
- Emotional resilience
- Open-mindedness
- A willingness to work as part of team
- Good IT and record keeping skills
- A willingness to undertake training and develop skills
For more information:
NHS Health Careers: Social Prescribing Link Worker
The NHS Health Careers page on social prescribing link workers (SPLWs).
To read it, please click here.
Are there any requirements to receive ARRS funding?
As noted under ‘Is funding available for them?‘, social prescribing link workers (SPLWs) can be reimbursed via the Additional Roles Reimbursement Scheme (ARRS). However, to be eligible for this funding, there are requirements that SPLWs must adhere to.
For instance, as stated in Annex B of the Network Contract Directed Enhanced Service contract specification 2021 / 22:
- “B3.3. Where a PCN employs or engages one or more Social Prescribing Link Workers under the Additional Roles Reimbursement Scheme or sub-contracts provision of the social prescribing service to another provider, the PCN must ensure that each Social Prescribing Link Worker providing the service has the following key responsibilities in delivering the service to patients:
- as members of the PCN’s team of health professionals, take referrals from
the PCN’s Core Network Practices and from a wide range of agencies to
support the health and wellbeing of patients; - assess how far a patient’s health and wellbeing needs can be met by
services and other opportunities available in the community; - co-produce a simple personalised care and support plan to address the
patient’s health and wellbeing needs by introducing or reconnecting
people to community groups and statutory services, including weight
management support and signposting where appropriate and it matters to the person; - evaluate how far the actions in the care and support plan are meeting the
patient’s health and wellbeing needs; - provide personalised support to patients, their families and carers to take
control of their health and wellbeing, live independently, improve their
health outcomes and maintain a healthy lifestyle; - develop trusting relationships by giving people time and focus on ‘what
matters to them’; - take a holistic approach, based on the patient’s priorities and the wider
determinants of health; - explore and support access to a personal health budget where
appropriate; - manage and prioritise their own caseload, in accordance with the health
and wellbeing needs of their population; and - where required and as appropriate, refer patients back to other health
professionals within the PCN.”
- as members of the PCN’s team of health professionals, take referrals from
For more information:
Network Contract DES contract specification 2021 / 22
Provided by NHSE / I, this document outlines the Network Contract Directed Enhanced Service (DES) for 2021 / 22.
To read it, please click here.
What clinical supervision do they need?
As noted in the Network Contract Directed Enhanced Service contract specification 2021 / 22, a primary care network (PCN) should provide a GP supervisor for the social prescribing link worker(s) (SPLWs).
NHS England & NHS Improvement (NHSE / I) elaborate on the specifics of this supervision in their induction guide, as follows:
“Your PCN will appoint a GP supervisor to provide direct supervision for your work. They will meet you regularly, provide line management, address any issues or concerns and help you to succeed in the role. This will include ensuring that you can raise patient-related concerns (such as abuse, domestic violence, or other safeguarding issues) and can refer individuals back to other health professionals as relevant, for further support, review or monitoring.
Where social prescribing link workers are employed by a partner ‘social prescribing provider’ agency, the GP supervisor will still be required. In this arrangement, the GP supervisor will also need to involve the partner organisation in regular progress updates about your role, enabling clear lines of accountability, effective, seamless, joint working and problem-solving challenges together.”
The guide also adds, separate from having a GP supervisor, that:
“As well as the ongoing support you will receive from the GP supervisor, you should have regular access to clinical or non-managerial supervision both with your GP supervisor and other relevant health professionals within the PCN. This ‘clinical’ or non-managerial supervision will help you to manage the emotional impact of your work and be guided by clinicians on dealing effectively with patient risk factors.”
For more information:
Induction Guide for Social Prescribing Link Workers
Provided by NHS England & NHS Improvement (NHSE / I), this document serves an induction guide for social prescribing link workers (SPLWs) starting employment in a primary care network.
To read it, please click here.
What should practice induction include?
Conveniently, NHS England & NHS Improvement (NHSE / I) have put together an induction guide for social prescribing link workers joining a primary care network. This seventeen-page document can signpost you to a range of resources and covers the following topics:
- Why does social prescribing matter?
- Who do you work for — and what is a primary care network?
- What will be you be doing as a social prescribing link worker?
- And more…
For more information:
Induction Guide for Social Prescribing Link Workers
Provided by NHS England & NHS Improvement (NHSE / I), this document serves an induction guide for social prescribing link workers (SPLWs) starting employment in a primary care network.
To read it, please click here.
What ongoing support is available for SPLWs?
NHS England & NHS Improvement (NHSE / I) have, in their social prescribing link worker (SPLW) induction guide, compiled a list of available support structures and mechanisms — including an online learning community, accessible by contacting england.socialprescribing@nhs.net.
The Hub's SPLW Lead
Our Profession Lead for Social Prescribing Link Workers (SPLWs) is Jeannie Morrice, here to provide a point of contact for this role, help set objectives and career goals, and to keep you in the loop with SPLW-related work.
Jeannie can be contacted at jeannie.morrice@nhs.net using the button below.
NHSE / I Services
Included in their induction guide for social prescribing link workers (SPLWs), NHS England & NHS Improvement (NHSE / I) have compiled a list of ongoing support and resources, including:
- Learning, developmental and peer support
- Regional learning co-ordinators
- Online link worker learning
- Online collaboration
To read it, please click here.
Example Job Description?
Health Education England (HEE) have not yet produced a template job description. Please check back for future updates.
What supervision do I need to provide?
See technical annexe
What Training & Development is available for SPLW?
Training and support from NHSE/I & HEE:
- NHSE/I list their support offers for PCN link workers here: https://www.england.nhs.uk/personalisedcare/social-prescribing/support-and-resources/
- Welcome & induction pack for SPLWs: https://www.england.nhs.uk/wp-content/uploads/2019/09/social-prescribing-link-worker-welcome-pack-web-2.pdf
- Mandatory accredited e-learning for SPLWs: https://www.e-lfh.org.uk/programmes/social-prescribing/
- NHSE/I have a social prescribing ‘workspace’ on FutureNHS (https://future.nhs.uk/socialprescribing/grouphome). This platform has information for new starters, links to e-learning, and discussion forums. Email england.socialprescribing@nhs.net to request access to this workspace.
- NHSE/I run fortnightly webinars on hot topics for SPLWs, accessible via FutureNHS. There is also a page signposting further training e.g. in personalised care, mental health & wellbeing, safeguarding and children & young people: https://future.nhs.uk/socialprescribing/view?objectID=22956656
Training & Support from the BNSSG Training Hub:
- BNSSG Training Hub has worked with the 6 locality VCSE anchor organisations to create peer support groups for SPLWs. All BNSSG PCN link workers have been invited to attend their local group. The peer support groups started in summer 2020 and are currently running once a month. Please contact sarah.ballisat@nhs.net for more information
- The BNSSH Training Hub have a SPLW Professional Lead to support SPLWs working in primary care in BNSSG and their employing PCNs. Our SPLW Lead is Jeannie Morrice, jeannie.morrice@nhs.net
Personalised care training:
The recommended training for SPLWs is as follows:
- The e-learning modules on personalised care on the Personalised care institute website: https://www.personalisedcareinstitute.org.uk/your-learning-options/
(Modules include: Core skills, Shared Decision Making, Personalised Care & Support Planning, Person Centred Approaches)
- Plus 2 day health coaching training, the training providers can be found on the link below, funding will need to be accessed via your employer. https://www.person alisedca reinstitute.org.uk/accredited-training/
Please note the BNSSG Training Hub are hoping to provide an accredited 2-day health coaching course from Spring/Summer 2022
Initial Support
See technical annexe for induction
Previous experience required?
There are no set entry requirements for this role because your life experience, personal qualities and values are generally more important than qualifications.
Some employers may ask for basic numeracy and literacy plus some IT skills and relevant work experience. Some may also require a qualification at level 3.
Once in a role, you will receive training and development to support you.
Health Careers Webpage
Pleased full details of requirements etc on the health careers site: Social prescribing link worker | Health Careers
The DES Role Descriptors
Below is the Network DES particulars for the SPLW role:
The Network Contract DES provides reimbursement for three personalised care roles based in primary care: Social Prescribing Link Workers, Health and Wellbeing Coaches and Personalised Care Coordinators. These roles form a resource for GPs and other primary care professionals to provide an all-encompassing approach to personalised care. In the context of the COVID-19 outbreak, these roles can also play a vital role in maintaining the health and wellbeing of those otherwise at risk of loneliness and social isolation. A single point of access is required for these roles to ensure that people receive the right support at the right time and to reduce the burden on general practice. This would generally be via the Social Prescribing Link Worker(s) who work with the other two roles to triage referrals.
8.5.2. A PCN’s Core Network Practices must identify a first point of contact for each Social Prescribing Link Worker, Health and Wellbeing Coach and Care Coordinator, in order to provide general advice and support, and (if different) a GP to provide supervision. This can be one or more named individuals within the PCN. Individual and group coaching supervision for the Health and Wellbeing coach role must also be available from a suitably qualified or experienced health coaching supervisor.
8.5.3. A PCN’s Core Network Practices must ensure the Social Prescribing Link Worker(s), Health and Wellbeing Coach(es) and Care Coordinator(s) can discuss patient related concerns and be supported to follow appropriate safeguarding procedures (e.g. abuse, domestic violence and support with mental health) with a relevant GP. This GP may be the patient’s named accountable GP, or another GP within the relevant Core Network Practice as appropriate.
8.5.4. Supporting guidance providing further information to help PCNs employ or engage Social Prescribing Link Workers, Health and Wellbeing Coaches and Care Co-ordinators is available at: a. Social prescribing link workers
Network Contract DES
Full details can be read here:
Finance & Network DES
Below is the Network DES particulars for the SPLW role:
The Network Contract DES provides reimbursement for three personalised care roles based in primary care: Social Prescribing Link Workers, Health and Wellbeing Coaches and Personalised Care Coordinators. These roles form a resource for GPs and other primary care professionals to provide an all-encompassing approach to personalised care. In the context of the COVID-19 outbreak, these roles can also play a vital role in maintaining the health and wellbeing of those otherwise at risk of loneliness and social isolation. A single point of access is required for these roles to ensure that people receive the right support at the right time and to reduce the burden on general practice. This would generally be via the Social Prescribing Link Worker(s) who work with the other two roles to triage referrals.
8.5.2. A PCN’s Core Network Practices must identify a first point of contact for each Social Prescribing Link Worker, Health and Wellbeing Coach and Care Coordinator, in order to provide general advice and support, and (if different) a GP to provide supervision. This can be one or more named individuals within the PCN. Individual and group coaching supervision for the Health and Wellbeing coach role must also be available from a suitably qualified or experienced health coaching supervisor.
8.5.3. A PCN’s Core Network Practices must ensure the Social Prescribing Link Worker(s), Health and Wellbeing Coach(es) and Care Coordinator(s) can discuss patient related concerns and be supported to follow appropriate safeguarding procedures (e.g. abuse, domestic violence and support with mental health) with a relevant GP. This GP may be the patient’s named accountable GP, or another GP within the relevant Core Network Practice as appropriate.
8.5.4. Supporting guidance providing further information to help PCNs employ or engage Social Prescribing Link Workers, Health and Wellbeing Coaches and Care Co-ordinators is available at: a. Social prescribing link workers – https://www.england.nhs.uk/publication/social-prescribing-link-workers
This can be found in the Network DES contract document, in chapter 8: Document template (england.nhs.uk)
Here is a reference guide, provided by NHS England which is aimed at primary care for the social prescribing link worker role:
Finance and DES-supported roles
This can be found in the Network DES contract document, in chapter 8: Document template (england.nhs.uk)
Here is a reference guide, provided by NHS England which is aimed at primary care for the social prescribing link worker role:
NHS England report template – data iconB0431-network-contract-des-specification-pcn-requirements-and-entitlements-21-22
Network Contract Links
This can be found in the Network DES contract document, in chapter 8: Document template (england.nhs.uk)
Here is a reference guide, provided by NHS England which is aimed at primary care for the social prescribing link worker role:
NHS England report template – data iconB0431-network-contract-des-specification-pcn-requirements-and-entitlements-21-22
Finance and DES-supported roles
This can be found in the Network DES contract document, in chapter 8: Document template (england.nhs.uk)
Here is a reference guide, provided by NHS England which is aimed at primary care for the social prescribing link worker role:
NHS England report template – data iconB0431-network-contract-des-specification-pcn-requirements-and-entitlements-21-22
Personalised Institute training links
SPLW Ref Guide
Health Careers Website Link
Health Careers Webpage
Pleased full details of requirements etc on the health careers site: Social prescribing link worker | Health Careers
NHSE Case Study
The above case study was found here: NHS England » A primary care navigator helped John to get his life back and address his ongoing health and social needs
Literature
Induction Guide for Social Prescribing Link Workers
Provided by NHS England & NHS Improvement (NHSE / I), this document serves an induction guide for social prescribing link workers (SPLWs) starting employment in a primary care network.
To read it, please click here.
Network Contract DES contract specification 2021 / 22
Provided by NHSE / I, this document outlines the Network Contract Directed Enhanced Service (DES) for 2021 / 22.
To read it, please click here.
NHSE / I Case Studies
Provided by NHS England & NHS Improvement (NHSE / I), this webpage features a wealth of case studies on social prescribing link workers.
To read it, please click here.
Network Contract Directed Enhanced Service: Additional Roles Reimbursement Scheme Guidance
Provided by NHS England & NHS Improvement (NHSE / I), this guidance document provides information on the Additional Roles Reimbursement Scheme (ARRS).
To read it, please click here.
NHSE / I Social Prescribing and Community-Based Support Summary Guide
Provided by NHS England & NHS Improvement (NHSE / I), this document is intended to outline what good social prescribing looks like and assist in implementing it.
To read it, please click here.
NHS Health Careers: Social Prescribing Link Worker
The NHS Health Careers page on social prescribing link workers (SPLWs).
To read it, please click here.
A / V resources
Social prescribing in practice: supporting social prescribing link workers
A series of short films produced by NSHE / I, exploring the impact that social prescribing can make on people, communities, and systems.
To watch it, please click here.
[This video was uploaded on 25.01.22.]